Leukorrhea: Expert Care for Complete Relief & Comfort
Noticing Unusual Vaginal Discharge? It Could Be Leukorrhea
Are you experiencing persistent vaginal discharge that feels unusual in color, smell, or quantity? While some discharge is normal and healthy, changes in its appearance or associated symptoms could indicate leukorrhea—a common condition affecting women during their reproductive years.
Abnormal discharge often brings discomfort, embarrassment, and anxiety. It can interfere with intimacy, lower confidence, and sometimes signal underlying infections or hormonal imbalances. Ignoring these signs can lead to complications like pelvic infections or reproductive issues.
The good news? Most cases of leukorrhea are treatable with accurate diagnosis and timely care.
At Vardaan Hospital, Dr. Dimple Doshi provides comprehensive evaluation and targeted treatment to restore comfort, health, and peace of mind—while also guiding you on preventive care for long-term wellness.
What Is Leukorrhea and Why Does It Happen?
Leukorrhea is a vaginal discharge that can be normal or indicate an infection. It occurs due to hormonal changes or infections like BV, yeast, or STIs.
- Normal discharge: Clear or white, mild odor
- Abnormal discharge: Thick, yellow-green, foul smell
- Causes include infection, pregnancy, poor hygiene
What Are the Symptoms of Vaginal Discharge or Leukorrhea?
Abnormal vaginal discharge may indicate infection if associated with foul odor, itching, pain, or color changes.
- Yellow, green, or curd-like discharge with odor
- Persistent wetness needing panty liners
- Vaginal itching or burning
- Lower abdominal pain or discomfort
- Burning during urination
- Pain during sexual intercourse
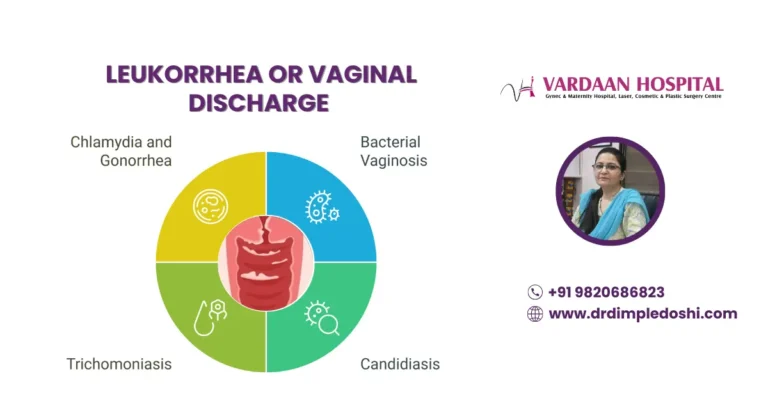
What Causes Vaginal Discharge or Leukorrhea?
Normal discharge can occur due to hormonal changes, while abnormal discharge is mostly due to infections or STIs.
- Normal Causes: Puberty, pregnancy, ovulation
- Abnormal Causes: Bacterial vaginosis, yeast infection, trichomoniasis, STIs like chlamydia and gonorrhea
What Are the Different Types of Vaginal Discharge?
Discharge type varies by infection and condition. Knowing these differences helps in early diagnosis and treatment.
- Bacterial Vaginosis: Thin, gray or green discharge, fishy odor
- Candidiasis: Thick white curdy discharge, severe itching
- Trichomoniasis: Frothy yellow-green discharge, foul smell
- Chlamydia & Gonorrhea: Pus-like discharge, painful urination
When Should You Worry About Vaginal Discharge?
Seek medical attention if discharge is smelly, colored, or associated with pain, itching, or urinary discomfort.
- Foul odor or green/yellow color
- Painful urination or burning sensation
- Lower abdominal pain or fever
How Is Leukorrhea Diagnosed?
Diagnosis includes history, physical examination, and lab tests to identify infection or hormonal imbalance.
- Gynecological examination
- Vaginal swab and culture tests
- Blood tests for infections and hormones
- Ultrasound if needed
How Is Leukorrhea Treated?
Treatment targets the underlying cause and includes antifungal, antibiotic, or probiotic therapy for infection control.
- Antibiotics for bacterial infections
- Antifungal medication for yeast infections
- Safe sexual practices to prevent recurrence
What Are the Possible Complications if Leukorrhea Is Untreated?
Ignoring symptoms can lead to serious reproductive health issues and infertility.
- Pelvic Inflammatory Disease (PID)
- Chronic pelvic pain
- Infertility or pregnancy complications
How Can Leukorrhea Be Prevented?
Good hygiene, safe sex, and proper care reduce the risk of recurrent infections and discharge.
- Maintain safe sexual practices
- Avoid douching and harsh cleaning products
- Wear breathable cotton underwear
- Avoid tight clothing for long hours
- Take probiotics during antibiotic treatment
Are Vaginal Washes Helpful or Harmful?
Use only pH-balanced, hypoallergenic washes when recommended by your doctor; avoid frequent douching.
- Reduces odor and discomfort in recurrent infections
- Overuse can disturb natural vaginal flora
What Is the Cost of Leukorrhea Treatment in Mumbai?
The cost varies based on infection type and diagnostic requirements. Average cost range in Mumbai:
- Consultation: ₹800 – ₹1000
- Lab Tests: ₹2000 – ₹5000
- Medications: ₹500 – ₹2000
Who Is the Best Doctor for Leukorrhea Treatment in Goregaon West?
Dr. Dimple Doshi at Vardaan Hospital offers expert care, accurate diagnosis, and personalized treatment plans for leukorrhea.
Which Is the Best Hospital for Leukorrhea Treatment in Mumbai?
Vardaan Hospital, Goregaon West, provides advanced diagnostic tools, comprehensive care, and an expert team for all gynecological issues.
Medical Code for Leukorrhea Treatment
ICD-10 Codes for Leukorrhea
| ICD-10 Code | Description |
|---|---|
| N89.8 | Other specified noninflammatory disorders of vagina (includes leukorrhea) |
| N89.9 | Noninflammatory disorder of vagina, unspecified |
| N76.0 | Acute vaginitis (often associated with discharge) |
| N76.1 | Subacute and chronic vaginitis |
| N76.9 | Unspecified vaginitis and vulvovaginitis |
CPT Codes for Leukorrhea Evaluation & Treatment
| CPT Code | Description |
|---|---|
| 99213 | Office or outpatient visit for evaluation and management (low complexity) |
| 99214 | Office or outpatient visit for evaluation and management (moderate complexity) |
| 87210 | Wet mount for infectious agents (saline or KOH prep) |
| 87070 | Bacterial culture, general (including vaginal pathogens) |
| 87510 | Molecular testing for vaginitis pathogens (Trichomonas, Candida, Gardnerella) |
| 96372 | Therapeutic injection (for antifungal or antibiotic treatment if needed) |
(FAQs) Frequently Asked Questions - Leukorrhea
Q1. How do I stop leukorrhea naturally?
Ans. Maintain good hygiene, wear breathable cotton underwear, avoid scented products, and consult your doctor for persistent cases.
Q2. Can stress cause leukorrhea?
Ans. Yes, stress can disrupt hormone balance, leading to increased vaginal discharge.
Q3. Which hormone causes leukorrhea?
Ans. Estrogen is the primary hormone responsible for normal vaginal discharge during the menstrual cycle and pregnancy.
Q4. Does leukorrhea smell?
Ans. Normal leukorrhea is odorless or mildly scented. A strong, foul smell may indicate infection and needs medical attention.
Q5. Why do I have a lot of leukorrhea?
Ans. It may result from hormonal changes, ovulation, pregnancy, or infections like bacterial vaginosis or yeast infection.
Q6. Can I get pregnant if I have leukorrhea?
Ans. Yes, leukorrhea is common during ovulation and pregnancy. However, infection-related discharge may affect fertility.
Q7. How does pregnancy discharge look compared to leukorrhea?
Ans. Pregnancy discharge is usually milky white and thicker, while normal leukorrhea is clear or slightly white.
Q8. What discharge indicates period is coming?
Ans. Creamy white discharge that thickens before your period is normal and indicates hormonal changes.
Q9. What color is leukorrhea in early pregnancy?
Ans. It is typically white or off-white, mild, and odorless during early pregnancy.
Q10. Is leukorrhea a sign of early pregnancy?
Ans. Yes, increased vaginal discharge can be an early pregnancy sign due to hormonal changes.
Q11. Can leukorrhea occur before a positive pregnancy test?
Ans. Yes, some women notice more discharge even before confirming pregnancy with a test.
Q12. Does white discharge mean period is coming or pregnancy?
Ans. White discharge before a missed period can indicate either. Only a pregnancy test can confirm.
Q13. How early can pregnancy discharge be detected?
Ans. Increased vaginal discharge may be noticeable within 1–2 weeks of conception.
Q14. What food should you avoid if you have leukorrhea?
Ans. Avoid overly spicy, oily foods and excess sugar, which can worsen infections linked to discharge.
Q15. What are the risk factors for leukorrhea?
Ans. Poor hygiene, infections, hormonal imbalance, stress, and unprotected sex can increase the risk.
Take charge of your health today.
Book your consultation with Dr. Dimple Doshi at
Vardaan Hospital, Goregaon West, Mumbai.


 WhatsApp
WhatsApp +91-9820686823
+91-9820686823 Book Appointment
Book Appointment