Hysteroscopy Surgery: Advanced & Safe Uterine Care in Mumbai
Struggling with Infertility or Abnormal Uterine Bleeding? Hysteroscopy Can Help
Are you facing repeated implantation failures, unexplained infertility, or abnormal uterine bleeding? These issues may be caused by hidden conditions like fibroids, polyps, adhesions, or a uterine septum—problems that often go undetected with regular scans.
Without accurate diagnosis, these conditions can silently affect your fertility and overall health. Many women undergo multiple treatments or IVF attempts without success because the underlying cause remains untreated. This not only delays motherhood but also creates emotional and financial stress.
Solution:
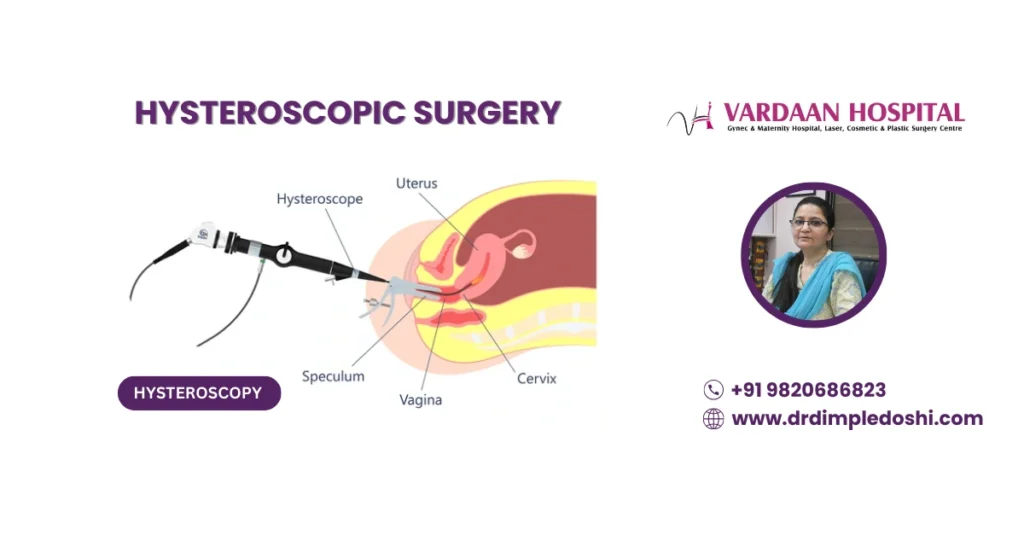
Hysteroscopy is a safe, minimally invasive procedure that uses a thin, lighted tube with a high-definition camera to examine and treat the uterine cavity. It requires no cuts, leaves no scars, and is performed as a daycare procedure—making it the gold standard for diagnosing and correcting issues like fibroids, polyps, adhesions, and uterine septa.
At Vardaan Hospital, Dr. Dimple Doshi specializes in advanced hysteroscopic procedures for women seeking fertility-friendly and precise treatment solutions.
Why Choose Hysteroscopy?
- Scarless, no incisions required
- Daycare procedure with minimal recovery time
- Ideal for infertility evaluation and treatment
- Corrects causes of abnormal bleeding and miscarriage risk
What Is Hysteroscopy Surgery?
Hysteroscopy is a minimally invasive gynecological procedure that uses a thin, lighted tube called a hysteroscope, connected to a high-definition camera. It allows direct visualization of the uterine cavity, helping gynecologists diagnose and treat conditions such as:
- Uterine fibroids
- Adhesions (Asherman’s syndrome)
- Polyps
- Septum
- Abnormal uterine bleeding
Why it’s preferred: Hysteroscopy is a safe, daycare procedure requiring no external cuts or stitches. It is scarless, offers faster recovery, and is highly effective for women with infertility or abnormal bleeding.
Synonyms / Related Terms
- Diagnostic hysteroscopy
- Operative hysteroscopy
- Minimally invasive uterine surgery
- Scarless uterine surgery
- Hysteroscopic uterine procedure
- Endoscopic uterine surgery
What Are the Types of Hysteroscopy Procedures?
Hysteroscopy is categorized into two main types based on the purpose of the procedure:
- Diagnostic Hysteroscopy: Used to examine the uterine cavity for conditions such as fibroids, polyps, adhesions, septum, and causes of infertility or abnormal bleeding. It can also include biopsy sampling.
- Operative Hysteroscopy: Performed to treat issues identified during diagnostic hysteroscopy. It involves using specialized instruments to remove fibroids, polyps, adhesions, uterine septum, or correct structural abnormalities.
Tip: Often, both diagnostic and operative procedures can be done in a single session, reducing the need for multiple surgeries.
When Is Hysteroscopy Needed?
Hysteroscopy is performed for both diagnostic and operative purposes. Here are the key indications:
Diagnostic Hysteroscopy
- Evaluating the uterine cavity in cases of infertility and collecting endometrial samples
- Investigating abnormal uterine bleeding or postmenopausal bleeding
- Diagnosing uterine septum, fibroids, adhesions, and polyps
- Performing a second-look hysteroscopy after previous surgery
Operative Hysteroscopy
- Septum removal (Septum resection or septoplasty): Corrects uterine septum for better fertility outcomes
- Submucosal fibroid removal: Improves uterine health and reduces heavy bleeding
- Adhesion removal: Treats intrauterine adhesions (Asherman’s syndrome) caused by infection, surgery, or D&C
- Tubal block correction: Opens blocked fallopian tubes for improved fertility
- Site-specific biopsy: Helps diagnose abnormal uterine or postmenopausal bleeding
- Isthmocele correction: Repairs C-section scar defects
- Cesarean scar ectopic removal: Removes pregnancy implanted on C-section scar
- Recurrent miscarriage evaluation: Identifies structural uterine issues
- Removal of lost IUD (Copper T): Safely extracts misplaced intrauterine devices
- Metroplasty: Corrects the shape of an abnormal uterus
Tip: Hysteroscopy offers precise treatment and diagnosis without external cuts, making it ideal for fertility management and abnormal bleeding cases.
What Conditions Can Be Diagnosed or Treated with Hysteroscopy?
Hysteroscopy provides a clear view of the uterine cavity, making it highly effective for diagnosing and treating various gynecological conditions, including:
- Abnormal Uterine Bleeding (AUB): Identifies causes like polyps, fibroids, or endometrial abnormalities
- Fibroids: Especially submucosal fibroids that affect bleeding and fertility
- Endometrial Polyps: Growths inside the uterine cavity that can cause irregular bleeding or infertility
- Intrauterine Adhesions (Asherman’s Syndrome): Scar tissue that interferes with normal menstruation and pregnancy
- Uterine Septum or Malformations: Structural abnormalities impacting conception and pregnancy outcomes
- Lost Intrauterine Device (IUD): Retrieval of misplaced contraceptive devices
- Causes of Infertility: Detects uterine factors affecting implantation and pregnancy
Tip: Hysteroscopy often combines diagnosis and treatment in one session, reducing the need for multiple procedures.
What Are the Benefits of Hysteroscopy Surgery?
Hysteroscopy offers several advantages over traditional surgical methods for diagnosing and treating uterine conditions. Key benefits include:
- Minimally invasive: No external cuts or stitches required
- Daycare procedure: Most patients go home the same day
- Minimal pain and quick recovery: Resume normal activities within a few days
- Accurate diagnosis: Provides a clear view of the uterine cavity for precise evaluation
- Effective treatment: Ideal for removing fibroids, polyps, adhesions, and correcting uterine septum
- Improves fertility: Restores normal uterine anatomy for better conception chances
- Alternative to hysterectomy: Treats certain conditions without removing the uterus
Tip: Hysteroscopy combines diagnosis and treatment in a single session, saving time and reducing complications.
Who Is the Right Candidate for Hysteroscopy Surgery?
Ideal candidates for hysteroscopy include women who:
- Have unexplained infertility or recurrent miscarriages
- Suffer from abnormal uterine bleeding
- Have uterine abnormalities like fibroids, polyps, or septum
- Need removal of intrauterine adhesions (Asherman’s syndrome)
- Require evaluation of the uterine cavity before IVF or ART
Tip: Your gynecologist will determine suitability based on symptoms, ultrasound, and medical history.
How Should You Prepare for a Hysteroscopy Procedure?
Proper preparation helps ensure a safe and smooth hysteroscopy experience. Here’s a pre-operative checklist:
- Schedule during the early menstrual phase: The uterine lining is thin, giving a clearer view
- Inform your doctor about medications: Especially blood thinners, diabetes, and thyroid drugs
- Fasting: Avoid food and water for 6–8 hours before the procedure if anesthesia is planned
- Pre-procedure tests: Blood work and imaging if advised by your doctor
- Avoid vaginal products: Stop using creams, douches, or tampons 24 hours before the procedure
- Arrange transport: Mild sedation or anesthesia may affect your ability to drive post-procedure
Tip: Follow all pre-op instructions given by your gynecologist for a smooth and complication-free experience.
How Is Hysteroscopy Performed Step by Step?
Hysteroscopy is a safe, minimally invasive procedure that combines diagnostic and therapeutic capabilities. Here’s how it is done:
- Anesthesia: Performed under short general anesthesia or mild sedation for patient comfort
- Duration: 8–10 minutes for diagnostic hysteroscopy and 15–20 minutes for operative hysteroscopy
Step-by-Step Procedure
- The uterine cavity is gently distended with sterile saline using a hysteromat system for controlled pressure and safety
- A thin hysteroscope with a high-definition camera is inserted through the cervix to visualize the uterine cavity
- A systematic examination of the uterus is performed to identify fibroids, polyps, septum, or adhesions
- If treatment is needed, specialized hysteroscopic instruments are used for removal or correction
- The procedure often concludes with a gentle D&C (dilation and curettage) for accurate diagnosis and tissue sampling
Tip: Hysteroscopy requires no external incision and is typically completed as a daycare procedure with a quick recovery.
What Happens Immediately After Hysteroscopy Surgery?
After hysteroscopy, you will be observed for a short period before discharge. Post-operative care typically includes:
- Recovery Time: Most patients can go home within a few hours
- Mild Symptoms: Light bleeding or mild cramping for 1–2 days
- Diet: Normal diet can be resumed within 2–4 hours
- Activity: Walking is encouraged; avoid strenuous exercise for 2–3 days
- Restrictions: No tampons or intercourse for at least 3–5 days
Tip: Contact your doctor immediately if you experience heavy bleeding, fever, or severe abdominal pain.
What Is the Recovery Timeline After Hysteroscopy Surgery?
Hysteroscopy is a daycare procedure with minimal downtime and quick recovery. Here’s what you can expect post-surgery:
- Hospital Stay: Daycare procedure; discharge within a few hours
- Diet: Resume normal diet 2–4 hours after the procedure
- Mobility: Start walking within 15 minutes to 1 hour
- Pain Level: Minimal or no pain; mild cramping in some cases
- Bathing: Allowed on the same day
- Follow-up: Scheduled after 5–6 days for review and reports
Tip: Avoid sexual intercourse, tampons, and strenuous activities for 3–5 days or as advised by your doctor.
What Are the Risks and Complications of Hysteroscopy?
Hysteroscopy is a safe, minimally invasive procedure, but like any surgery, it carries some rare risks. Possible complications include:
- Anesthesia-related risks: Mild reactions to sedatives or general anesthesia
- Excessive bleeding: Usually controlled during the procedure
- Fluid overload: From distension media used during the procedure
- Uterine perforation: Accidental puncture of the uterine wall (rare)
- Infection: Low risk if proper sterile techniques are followed
When to call your doctor: Severe abdominal pain, heavy bleeding, fever, or urinary problems after the procedure require immediate medical attention.
When Should You Avoid Hysteroscopy?
Hysteroscopy is generally safe, but it should be avoided in the following situations:
- Current pregnancy
- Active pelvic infection or untreated sexually transmitted infection (STI)
- Recent uterine perforation or major uterine surgery
- Severe medical instability or uncontrolled chronic illness
- Heavy uterine bleeding that prevents clear visualization
Tip: Always undergo a full evaluation before scheduling hysteroscopy to ensure safety.
What Is the Success Rate of Hysteroscopy in Treating Infertility and Uterine Problems?
Hysteroscopy is highly successful in improving fertility and treating uterine abnormalities. Success rates include:
- Infertility treatment: 50–70% success when combined with other fertility treatments
- Fibroid and polyp removal: Over 90% symptom relief and improved conception chances
- Adhesion removal: 80–90% restoration of normal uterine cavity
Fact: Studies show hysteroscopy significantly boosts IVF success rates by correcting intrauterine issues before embryo transfer.
What Is the Cost of Hysteroscopy Surgery in Goregaon West, Mumbai?
The cost of hysteroscopy surgery at Vardaan Hospital depends on the type of room and services selected. Here is an approximate price range:
- General Ward: ₹50,000
- Semi-Special Room: ₹68,000 – ₹75,000
- Deluxe Room: ₹1,20,000
- Super Deluxe Room: ₹1,50,000
- Suite Room: ₹2,00,000
Note: Final costs depend on the complexity of the procedure and additional services. For an accurate estimate, consult Dr. Dimple Doshi at Vardaan Hospital, Goregaon West, Mumbai.
Who Is the Best Gynecologist for Hysteroscopy in Mumbai?
Dr. Dimple Doshi is one of Mumbai’s leading gynecologists, renowned for her expertise in advanced hysteroscopic procedures. With decades of experience and thousands of successful cases, she specializes in:
- Diagnostic and operative hysteroscopy for fibroids, polyps, and uterine abnormalities
- Fertility-preserving procedures for women planning pregnancy
- Minimally invasive, scarless techniques with quick recovery
Practice Location: Vardaan Hospital, Goregaon West, Mumbai – a trusted center for advanced gynecological care.
Why Choose Vardaan Hospital for Hysteroscopy in Goregaon West, Mumbai?
Vardaan Hospital is a trusted center for advanced gynecological care. Here’s why it is the preferred choice for hysteroscopy:
- Expert Care: Dr. Dimple Doshi has extensive experience and has successfully performed thousands of hysteroscopic procedures
- Advanced Technology: Equipped with high-definition cameras and modern hysteroscopic instruments for precision
- Comprehensive Diagnosis & Treatment: Both diagnostic and operative hysteroscopy performed in a single sitting
- Daycare Procedure: Minimal downtime, same-day discharge, and fast recovery
- Patient-Centric Approach: Personalized care, transparent pricing, and dedicated support throughout the treatment
Tip: Choose a center with proven expertise for better outcomes and reduced complications.
Medical Codes for Hysteroscopy Surgery
ICD-10 Codes for Hysteroscopy Indications
| ICD-10 Code | Description |
|---|---|
| N84.0 | Polyp of corpus uteri (common indication for hysteroscopic removal) |
| N84.1 | Polyp of cervix uteri |
| N85.0 | Endometrial hyperplasia |
| N92.0 | Excessive and frequent menstruation with regular cycle |
| N93.8 | Other specified abnormal uterine and vaginal bleeding |
| N85.8 | Other specified noninflammatory disorders of uterus |
| Z31.41 | Encounter for fertility testing (diagnostic hysteroscopy) |
CPT Codes for Hysteroscopy Surgery
| CPT Code | Description |
|---|---|
| 58555 | Hysteroscopy, diagnostic (separate procedure) |
| 58558 | Hysteroscopy, surgical; with sampling (biopsy) of endometrium and/or polypectomy |
| 58559 | Hysteroscopy, surgical; with lysis of intrauterine adhesions (synechiae) |
| 58560 | Hysteroscopy, surgical; with removal of submucous myoma |
| 58561 | Hysteroscopy, surgical; with removal of intrauterine device |
| 58562 | Hysteroscopy, surgical; with endometrial ablation (thermal/electrical) |
| 58563 | Hysteroscopic endometrial ablation for abnormal uterine bleeding |
| 58340 | Introduction of catheter for hysterosalpingography (commonly combined with diagnostic hysteroscopy for infertility) |
FAQs for Hysteroscopy Surgery
Q1. Is hysteroscopy a major surgery?
Ans. No, hysteroscopy is a minimally invasive procedure and typically performed as an outpatient treatment with no overnight stay.Q2. Are there any stitches in a hysteroscopy?
Ans. No, hysteroscopy does not require any external incisions or stitches as the scope is inserted through the natural opening of the cervix.Q3. How much does a hysteroscopy cost in India?
Ans. The cost varies between ₹20,000 and ₹60,000 depending on the complexity, hospital facilities, and surgeon expertise.Q4. Can I get my period after a hysteroscopy?
Ans. Yes, your menstrual cycle generally returns to normal after the procedure, though the first period may be slightly heavier or delayed.Q5. Can you get pregnant after a hysteroscopy?
Ans. Yes, hysteroscopy can improve fertility by removing polyps, fibroids, or adhesions that interfere with conception.Q6. What happens after a hysteroscopy procedure?
Ans. Patients may experience mild cramping or spotting for a few days. Most can resume normal activities within 24–48 hours.Q7. Who needs a hysteroscopy?
Ans. Women with unexplained infertility, heavy bleeding, recurrent miscarriage, or suspected uterine abnormalities may require this procedure.Q8. Is hysteroscopy done without anesthesia?
Ans. Diagnostic hysteroscopy can often be done without anesthesia, while operative hysteroscopy typically requires sedation or general anesthesia.Q9. What type of doctor performs a hysteroscopy?
Ans. A gynecologist trained in minimally invasive surgery usually performs hysteroscopy.Q10. Is hysteroscopy painful after surgery?
Ans. Mild cramping or discomfort may occur after the procedure but is usually short-lived and manageable with simple pain relief.Q11. Can I climb stairs after a hysteroscopy?
Ans. Yes, light activities like climbing stairs are generally safe after the procedure unless your doctor advises otherwise.Q12. Which is more painful: HSG or hysteroscopy?
Ans. Hysteroscopy is often more comfortable than HSG as it is done under local or general anesthesia for operative cases.Q13. Can hysteroscopy unblock fallopian tubes?
Ans. Hysteroscopy is primarily used for uterine issues; for blocked tubes, laparoscopy or other fertility procedures may be needed.Q14. Can hysteroscopy delay periods?
Ans. Yes, your first period after hysteroscopy might be slightly delayed due to hormonal and uterine recovery.Q15. Which is better: laparoscopy or hysteroscopy?
Ans. Both serve different purposes—hysteroscopy is for uterine evaluation, while laparoscopy examines the pelvic cavity and fallopian tubes.Q16. Is general anesthesia used for hysteroscopy?
Ans. Diagnostic hysteroscopy may not require anesthesia, while operative hysteroscopy usually needs sedation or general anesthesia.Q17. What are the restrictions after hysteroscopy?
Ans. Avoid intercourse, tampons, and strenuous activities for a few days or as directed by your doctor to prevent infection.Q18. How long should you rest after hysteroscopy?
Ans. Most women can resume normal routine within 24–48 hours, but complete recovery depends on the complexity of the procedure.Take charge of your health today.
Book your consultation with Dr. Dimple Doshi at
Vardaan Hospital, Goregaon West, Mumbai.


 WhatsApp
WhatsApp +91-9820686823
+91-9820686823