Uterine and Cervical Polyps: Causes, Symptoms, and Treatment
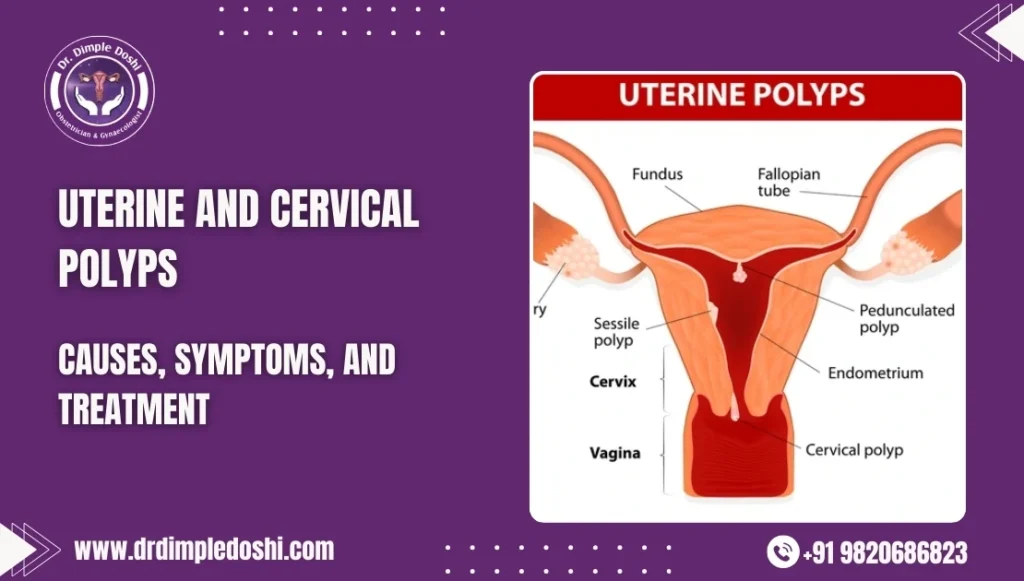
Table of Contents
Introduction
Uterine and cervical polyps are soft, spongy, and sometimes firm growths that may appear cherry-red, reddish-purple, or greyish-white in color. These growths can develop inside the uterus, where the baby grows, or may extend out through the cervix, sometimes becoming visible outside the vagina. Simply put, they are an overgrowth of uterine tissue.
Types of Uterine Polyps
There are two primary types of polyps that grow in the uterus:
- Endometrial or Uterine Polyps: These develop inside the uterine cavity.
- Cervical Polyps: These grow in the cervix and can be categorized further into:
- Endocervical Polyps: Develop inside the cervix.
- Ectocervical Polyps: Grow on the outer part of the cervix.
Causes of Uterine Polyps
Several factors contribute to the development of uterine polyps, including:
- Abnormal estrogen response: Overgrowth of the endometrium in a particular area.
- Chronic infection and inflammation: Persistent inflammation of the uterine lining can lead to polyp formation.
- Excessive fat and obesity: High estrogen levels from excess fat can stimulate polyp growth.
- Hypertension: Studies show a link between high blood pressure and polyp development.
- Menopause and aging: Hormonal changes during these phases trigger polyp growth.
- PCOD (Polycystic Ovarian Disease): Known to cause hormonal imbalances that can lead to polyps.
- Certain medications: Tamoxifen, a drug used in breast cancer treatment, can cause polyp formation and endometrial hyperplasia.
Diagnosis of Uterine Polyps
Doctors diagnose uterine polyps using various methods:
- Physical Examination: Can detect externally visible cervical polyps or protruding endometrial polyps.
- Ultrasonography: Helps identify endometrial polyps inside the uterus.
- Hysteroscopy: A direct visualization technique to accurately diagnose polyps.
- Biopsy (D&C): Sometimes polyps are found in a biopsy taken during dilation and curettage (D&C).
Symptoms of Uterine Polyps
Many polyps do not cause symptoms, especially small ones. However, when symptoms do appear, they include:
- Irregular bleeding
- Prolonged spotting
- Intermenstrual bleeding (bleeding between periods)
- Post-coital bleeding (bleeding after sexual activity)
- Persistent vaginal discharge and infection
- Heavy menstrual bleeding
- Postmenopausal bleeding
- Pain and discomfort during intercourse
Treatment of Uterine Polyps
- Observation: Small, asymptomatic polyps do not require treatment but should be monitored with regular ultrasounds.
- OPD Removal: Externally visible cervical polyps (ectocervical polyps) can be removed in an outpatient setting without anesthesia.
- Hysteroscopic Polypectomy: The most effective and minimally invasive procedure for removing uterine polyps, ensuring complete removal under magnification.
- D&C (Dilation and Curettage): A blind procedure that removes the polyp along with the uterine lining.
- Medications: Limited role in polyp removal, but progesterone tablets and GnRH agonists can help shrink small polyps temporarily by counteracting estrogen effects.
Prevention of Uterine Polyps
Preventing uterine polyps involves simple lifestyle and healthcare measures:
- Maintain a healthy lifestyle: Obesity increases the risk of diabetes, high blood pressure, and polyp formation.
- Regular gynecological check-ups: Polyps often develop silently without symptoms, making routine exams crucial.
- Prevent STDs: Sexually transmitted diseases can cause infections and inflammation, which may contribute to polyp formation.
Conclusion
Uterine and cervical polyps are common but manageable growths. Early detection through routine check-ups and proper treatment can help prevent complications. Maintaining a healthy lifestyle and being aware of symptoms ensures better reproductive health for women. If you experience unusual bleeding or other symptoms, consult a gynecologist promptly for proper diagnosis and treatment.

